InfoComm: Diagnosing the Healthcare AV Market
This column was reprinted with permission from InfoComm International.
What’s the fastest-growing market for AV systems in North America? Healthcare, according to InfoComm’s latest Market Definition and Strategy Study. There are a couple reasons for this. One has to do with the nature of the healthcare market itself; the other with the enabling power of AV.
By all accounts, healthcare is poised for continued growth, especially as baby boomers age. That doesn’t necessarily mean new hospitals will be sprouting up all over the United States. If anything, the country already has plenty of hospital beds, according to Kate Berry, CEO of the National eHealth Collaborative (NeHC). NeHC is a partner in InfoComm’s first-ever healthcare conference, in November.
What the market needs, Berry says, are alternative ways of delivering healthcare, including new outpatient centers, which serve to push healthcare closer to the people who need it and prevent taxing hospitals with non-emergencies. “There’s a trend to delivering more care outside the hospital than inside the hospital,” she says. Those new centers, like any professional office building these days, need AV systems, from digital signage to videoconferencing systems.
Which leads to the second reason healthcare is a growing market for AV: All healthcare facilities — new and old — benefit from the new applications that AV systems enable. Telemedicine is one of the most prominent, thanks in part to ongoing government funding of videoconferencing gear in rural clinics, but also to the fact that telemedicine spans so many applications.
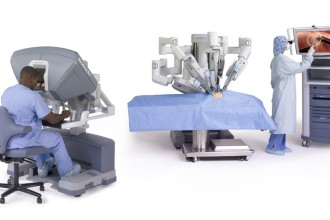
“We are seeing a few trends develop within telemedicine,” says Jim Hatcher, chief technology officer of Human Circuit, which targets the healthcare market. “One is interventional consultation — specialists scheduling time to consult via video teleconference. Many hospitals have telemedicine rooms specifically for interventional consultation during a surgical procedure or diagnoses. Very common in radiology.”
Two other trends, Hatcher says, are video links between paramedics in the field and specialists in other locations, such as hospitals, as well as simpler doctor-patient consultations. Those consultations sometimes extend to a patient’s home as part of an effort to bring care to patients instead of patients always traveling to a place of care. Although AV integrators aren’t usually the ones installing the in-home components, the trend bears watching because it affects what goes into a hospital or physician’s office.
In general, because of the nature of doctor-patient communications (i.e., between an office and a home), electronic-consultation solutions will have to support videoconferences with consumer endpoints, such as Skype or Google Talk—something not easily accomplished these days. The need for that kind of consumer-pro interoperability could favor cloud-based solutions, such as those from Blue Jeans Network and Vidtel.
Consumer-pro interoperability may also prove useful for medical school video applications, where student endpoints are unlikely to include Polycom or Cisco codecs, but rather web cams. The University of Central Florida College of Medicine, for example, is considering such a cross-platform system so that third- and fourth-year students at hospitals can be connected to the campus.
“It’s a way for the students to be able to conference back into the classrooms,” says Michael Reaves, the school’s director of systems engineering.
But keep in mind, say experts: What sells well in a teaching hospital isn’t necessarily a slam-dunk in the hospital. Understanding the ultimate customer, as always, is key to pitching the right proposal.
“We see all benefitting from video that captures team interaction and is intended to provide situational awareness and team improvement,” says Human Circuit’s Hatcher. “However, video designed to capture a procedure tends to be limited to teaching hospitals. There is a reluctance to capture a procedure on video due to the possibility of litigation. Often doctors are advised not record their procedures for fear of litigation.”
More, Bigger Med Schools
The University of Central Florida College of Medicine is a rarity. Founded in 2006, it’s one of only a handful of new U.S. medical schools. The passage of the Affordable Care Act has many pundits speculating that the newly insured masses will lead to an acute physician shortage over the next several years. In response, additional schools might open, while existing ones might expand. Either way, it would grow the market for healthcare AV.
The University of Missouri is an example of a medical school that’s in expansion mode. Based in Columbia, the school is expanding to Springfield, about three hours away. The goal is to train about 50 additional students in collaboration with Mercy and Cox Hospital systems.
“We have an institutional simulation recording and assessment system in place that we plan on deploying to the Springfield campus,” says Chris Sanders, the school’s operations manager for the Russell D. and Mary B. Shelden Clinical Simulation Center. “Physicians should be able to collaborate synchronously and asynchronously using the current learning management system and underlying AV technologies.”
Simulation systems span everything from “task trainers” – for example, an electronic human head, in the case of a dental school – to full-size mannequins that move and moan. The AV opportunity centers around capturing those training sessions.
“We see increasing use of simulation systems,” says Craig Park, principal consultant for The Sextant Group. “We see those kinds of labs being created in nursing schools and other kinds of allied health facilities, where the practice of working on this device is recorded using cameras and live audio, and then replayed to the class or the student.”
But keep in mind: Although medical schools often are synonymous with cutting-edge technology — including AV — that doesn’t mean they’re willing to be guinea pigs. Just the opposite.
“Universities want everything tested time and time again before we invest,” says Rachel Mutrux, director of the Missouri Telehealth Network.
The preference for proven technologies – including AV – isn’t limited to medical schools. In the case of emerging technologies, reviews and pilot projects could provide some of that proof, but it’s likely that regulators and prospective customers will want something deeper.
“I think those reviews and pilots are one thing, but the FDA is really wanting studies paid for by an unbiased organization that is going to have a control group and test group,” Mutrux says. “They’re going to measure the real efficacy of these designs.”
Beyond AV
In the enterprise market, some AV pros have expanded into building automation and management in order to capitalize on customer interest in saving energy. The healthcare market offers similar opportunities to branch out. For example, hospitals are increasingly using radio frequency identification (RFID) tags and scanners for tracking equipment, medication and even patients. RFID systems linked to AV systems may help facilitate care.
“By using building-automation tools such as AMX’s RMS and Crestron’s Fusion, sets of situations can be triggered to program a room for that patient,” says Sextant Group’s Park.
In building automation and management, one challenge for AV integrators are client fiefdoms that don’t want to share control over HVAC and other building systems. Resistance and skepticism can be even stronger in healthcare, something AV pros need to be prepared for if they want to branch into other medical systems.
“You have a long history of silos in the healthcare industry that will delay — not prohibit — that kind of integration,” Park says. “How fast that happens has a lot to do with the acceptance of that metacontrol model in other industries. The key word in healthcare planning these days is ‘evidence-based design.’ Until you can prove it’s better, it’s likely to be slow in acceptance.”
No Rush to Revenue
So what does it take to be successful in healthcare AV? Some factors might come as a surprise, especially when they have nothing to do with technology. Case in point: the ability to manage cash flow. Healthcare AV projects typically take longer than most other verticals. AV pros need to understand this and adjust their processes (and expectations) accordingly,
“If it’s a new build, it’s definitely a long sales cycle — between two and three years,” says Mary Glimm, AVI-SPL’s director of healthcare sales.
A common reason for that lead time is the amount of people and disciplines involved.
“You better be ready to be involved with multiple disciplines,” says Matt Oswalt, president of VIZIONefx, an integrator that targets the healthcare market. “AV, media services and IT might be the people spearheading it, but there may be 10 or 15 other decision-makers. As much as money, that’s what drags out the sales cycle.”
But there are exceptions, such as when a hospital has a marquee surgeon whose local or national reputation brings in a lot of business. “If those types of doctors want something, it moves very fast,” Glimm says.
“Hospitals, teaching hospitals and surgery centers are all in competition with each other,” says Human Circuit’s Hatcher. “Often AV technology and telemedicine facilities will attract talent and ultimately help the bottom line.”
Glimm agrees: “The new physicians like technology – a lot.”
Despite all the hoopla over how much the U.S. government and citizens spend on healthcare, it’s a mistake to assume that hospitals, physicians groups and other providers have plenty to spend on AV. In reality, budgets often are barriers to adoption. As a result, another success factor is indentifying the applications and specialties where budgets tend to be bigger.
“The main hurdle is finances,” Oswalt says. “Eighty percent of the hospitals in this country are losing money. The nice thing is that there’s a lot of mandating going on from governments to educate patients before they go home. There is a pool of money that hospitals have to dedicate to that.”